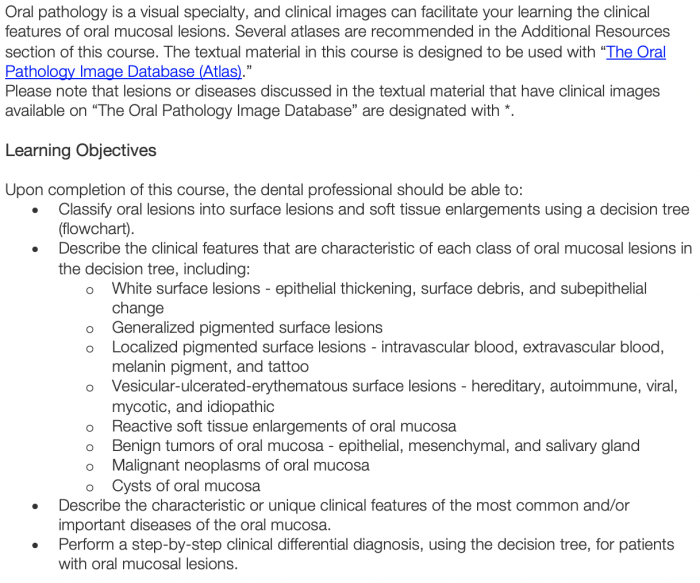
A Guide to Clinical Differential Diagnosis of Oral Mucosal Lesions provides a comprehensive framework for clinicians to navigate the complexities of diagnosing oral mucosal lesions. This guide empowers healthcare professionals with the knowledge and tools necessary to accurately identify and differentiate various oral mucosal lesions, leading to optimal patient outcomes.
Oral mucosal lesions encompass a wide spectrum of clinical presentations, posing diagnostic challenges. This guide addresses these challenges by presenting a systematic approach to differential diagnosis, incorporating clinical examination, history taking, diagnostic tests, and a comprehensive classification system. By integrating these elements, clinicians can effectively distinguish between common and uncommon oral mucosal lesions, ensuring appropriate management and treatment.
1. Overview of Oral Mucosal Lesions: A Guide To Clinical Differential Diagnosis Of Oral Mucosal Lesions
Oral mucosal lesions are any abnormalities or changes in the appearance of the soft tissues lining the oral cavity, including the lips, cheeks, tongue, gums, and palate.
Clinical differential diagnosis is crucial for identifying and distinguishing between various types of oral mucosal lesions, as they can have different etiologies, prognoses, and treatment approaches.
Diagnosing oral mucosal lesions can be challenging due to the wide range of clinical presentations and the potential for overlapping features among different conditions.
2. Classification of Oral Mucosal Lesions
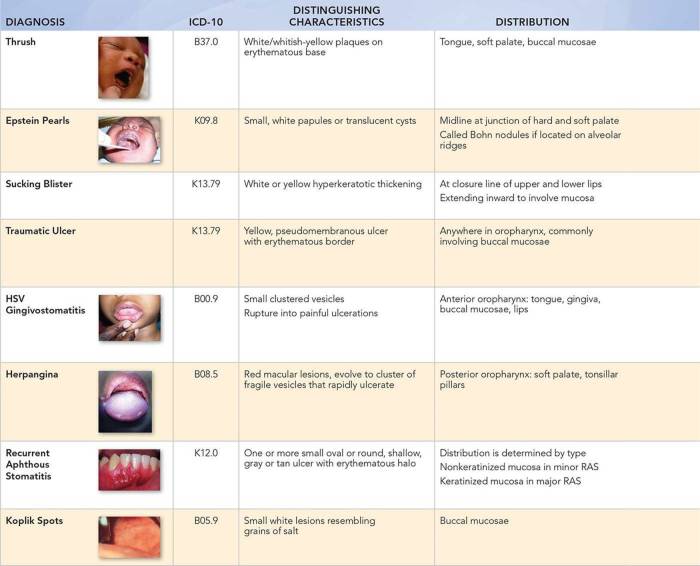
Oral mucosal lesions can be classified based on their clinical presentation, etiology, or histopathological features.
One comprehensive classification system categorizes oral mucosal lesions into the following groups:
| Group | Description |
|---|---|
| Inflammatory lesions | Lesions caused by inflammation, such as aphthous ulcers, lichen planus, and candidiasis |
| Infectious lesions | Lesions caused by infections, such as herpes simplex virus, human papillomavirus, and syphilis |
| Neoplastic lesions | Lesions with abnormal cell growth, including benign tumors (e.g., fibromas) and malignant tumors (e.g., squamous cell carcinoma) |
| Traumatic lesions | Lesions caused by physical trauma, such as lacerations, abrasions, and burns |
| Developmental lesions | Lesions present from birth or early childhood, such as geographic tongue and white sponge nevus |
3. Clinical Examination and History Taking

A thorough clinical examination is essential for diagnosing oral mucosal lesions.
The examination should include:
- Visual inspection of the oral cavity
- Palpation of the lesions to assess their texture, consistency, and mobility
- Assessment of the surrounding tissues and any associated symptoms
Obtaining a detailed patient history is also crucial.
Relevant questions to ask include:
- When did the lesion first appear?
- Have you had similar lesions in the past?
- Do you have any pain or discomfort associated with the lesion?
- Have you noticed any changes in the size, shape, or color of the lesion?
- Are there any other symptoms, such as fever, fatigue, or difficulty swallowing?
General Inquiries
What is the significance of clinical differential diagnosis in oral mucosal lesions?
Clinical differential diagnosis plays a crucial role in identifying the underlying cause of oral mucosal lesions, guiding appropriate treatment, and preventing potential complications.
What are the common challenges encountered in diagnosing oral mucosal lesions?
Diagnosing oral mucosal lesions can be challenging due to their diverse clinical presentations, overlapping features, and the need for specialized knowledge and expertise.
How does this guide assist in the management of oral mucosal lesions?
This guide provides a comprehensive overview of management strategies for different types of oral mucosal lesions, including treatment options, factors to consider, and interdisciplinary collaboration.